Abstract
Background: The thalassemias are a group of red blood cell (RBC) disorders in which ineffective erythropoiesis and hemolysis occur due to imbalanced production and precipitation of globin chains. Thalassemic RBCs have insufficient levels of ATP to meet increased energy demands associated with globin chain imbalance, protein degradation, and cellular oxidative stress responses. Mitapivat (AG-348) is a first-in-class, small-molecule, oral activator of RBC pyruvate kinase (PKR), a key enzyme regulating ATP production via glycolysis. In a phase 2, open-label trial of mitapivat in adults with α- or β-non-transfusion-dependent (NTD) thalassemia (NCT03692052), 80.0% (16/20) of patients (pts) met the primary endpoint of a hemoglobin (Hb) response (increase ≥ 1.0 g/dL from baseline at 1 or more assessments between Wks 4-12, inclusive). Improvements in markers of hemolysis and erythropoiesis were also observed in pts and mitapivat was generally well tolerated.
Methods: Pts aged ≥ 18 (yrs) with a known medical history of α- or β-thalassemia, Hb concentration of ≤ 10.0 g/dL, and ≤ 5 RBC units transfused in prior 24 wks and none in 8 wks prior to study drug were eligible for the study. All pts started mitapivat at 50 mg twice daily (BID), escalating to 100 mg BID based on individual safety and Hb assessments. After completion of the 24-wk core period, pts were continued on mitapivat treatment in the extension period if they had achieved a Hb response, or a delayed Hb response (Hb increase of ≥ 1.0 g/dL at ≥ 1 assessment after Wk 12), with no ongoing grade ≥ 3 treatment-emergent adverse events (AE) related to study drug. Eligible pts continued mitapivat at the dose received at their Wk 24 visit. Study visits are conducted every 12 wks and will continue for up to 10 yrs. The extension period of the study is ongoing, here we report data up to Wk 72 visit (data cutoff March 27, 2021).
Results: Of the 19 pts who completed the core period, 17 entered the extension period. During the extension period, 16 pts received 100 mg BID mitapivat and 1 received 50 mg BID. As of the cutoff date, 1 pt had discontinued (patient decision). Median (range, in wks) duration of mitapivat treatment for pts who entered the extension period was 70.9; (54.7, 105.6), with 8 of 17 pts receiving 72 wks or more of treatment as of the cutoff date for this analysis. The Median age of pts who entered the extension period was 44 yrs (range 29, 67). Mean baseline (standard deviation [SD]) Hb, total bilirubin and lactate dehydrogenase (LDH) was 8.1 (1.2) g/dL, 40.1 (26.2) μmol/L and 272.4 (121.7) U/L, respectively. Median baseline erythropoietin (EPO) was 70.5 (range 15, 11191) IU/L.
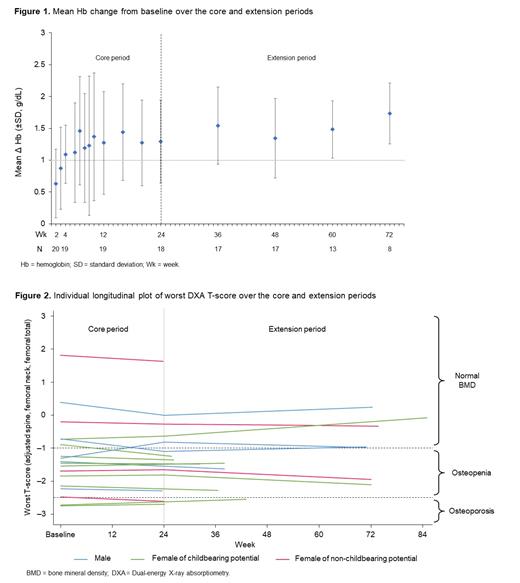
Improvements in Hb concentration achieved in the core period were sustained in the extension study (n = 8 at Wk 72; Figure 1). Mean Hb (SD) increase from baseline to Wk 60 (which includes 4 pts with α- and 9 with β-thalassemia) and Wk 72 (which includes 8 pts with β-thalassemia) were 1.5 (0.4) g/dL and 1.7 (0.5) g/dL, respectively. Improvements in markers of hemolysis and ineffective erythropoiesis observed in the core period were maintained in the extension period up to Wk 72 (mean [SD] bilirubin and LDH, -15.8 [16.6] μmol/L and -63.6 [216.0] U/L, respectively; median [range] EPO, -33.0 [-72.0, -16.0] IU/L).
The safety profile was consistent with that observed during the core period. AEs occurring in ≥ 15% of pts during the extension period were headache (5/17) and back pain (3/17), none of which were grade ≥ 3. No notable trends for changes in bone mineral density were observed (Figure 2). There were no treatment-related serious AEs during the extension period.
Conclusions: In pts with either α- or β-thalassemia, a favorable efficacy-safety profile was observed with long-term treatment with mitapivat. Results show sustained improvements in Hb, hemolysis and ineffective erythropoiesis - despite the globin genotypic heterogeneity of the cohort - and no new safety findings. Mitapivat, through its unique mechanism of action, may represent a novel therapeutic approach for this condition. Two phase 3 trials of mitapivat in α- and β-thalassemia, one in pts who are NTD and one in pts who are transfusion-dependent, will be initiated in 2021.
Kuo: Bluebird Bio: Consultancy; Alexion: Consultancy, Honoraria; Agios: Consultancy, Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Honoraria; Apellis: Consultancy; Pfizer: Consultancy, Research Funding; Bioverativ: Membership on an entity's Board of Directors or advisory committees; Celgene: Consultancy. Layton: Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Agios Pharmaceuticals: Consultancy, Membership on an entity's Board of Directors or advisory committees; Cerus: Membership on an entity's Board of Directors or advisory committees. Lal: Chiesi: Consultancy; Agios Pharmaceuticals: Consultancy; bluebird bio, Inc.: Research Funding; La Jolla Pharmaceutical Company: Research Funding; Terumo Corporations: Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding; Insight Magnetics: Research Funding; Protagonist Therapeutics: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Research Funding. Al-Samkari: Dova/Sobi: Consultancy, Research Funding; Moderna: Consultancy; Argenx: Consultancy; Rigel: Consultancy; Amgen: Research Funding; Novartis: Consultancy; Agios: Consultancy, Research Funding. Bhatia: Agios Pharmaceuticals: Current Employment, Current equity holder in publicly-traded company. Kosinski: Agios Pharmaceuticals: Current Employment, Current equity holder in publicly-traded company. Tong: Agios Pharmaceuticals: Current Employment, Current equity holder in publicly-traded company. Lynch: Agios Pharmaceuticals: Current Employment, Current equity holder in publicly-traded company. Uhlig: Agios Pharmaceuticals: Current Employment, Current equity holder in publicly-traded company. Vichinsky: Agios Pharmaceuticals: Consultancy, Research Funding; Bluebird Bio: Consultancy, Research Funding; Global Blood Therapeutics: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal